Abstract
Polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (pMF) are three major components of myeloproliferative neoplasms (MPNs). They may be transformed to either secondary MF (sMF) or secondary acute myeloid leukemia (sAML). In addition, they can have second cancers during follow up (FU). It is important to understand the incidence rates and patterns of the transformation and second cancers because by the information we can understand clinical courses of MPNs holistically and figure out the actual socio-economic impact of MPNs on patients and communities.
South Korea has a compulsory National Health Insurance System (NHIS), covering ~97% of the population. Claims data from health care providers to NHIS are submitted to the Health Insurance Review and Assessment Service (HIRA) for reimbursement for a service provided to patients. Because claims data for the remaining ~3% of the population belonging to the National Medical Aid Program are also reviewed by HIRA, nationwide epidemiologic studies are feasible. We conducted an epidemiologic study to elucidate clinical course of MPNs patients focusing on disease transformation and second cancers by analyzing the HIRA database. Cumulative incidence (CI) of transformation or second cancer were calculated considering death as a competing risk.
A total of 7,471 patients (median age 60 years, range 11-106) who were diagnosed as one of the three kinds of MPNs from Jan. 2008 to Dec. 2016 and with appropriate F/U data for the analysis were included (4,405 for ET, 2,470 for PV, and 596 patients for pMF). Among ET patients (median F/U duration 46.7 months), 223 patients (5.06%) underwent any transformation during study period; ET→PV (i.e., initially diagnosed ET but changed to PV later; N = 80), ET→PV→sMF (N = 2), ET→PV→sAML (N = 1), ET→sMF (N = 68), ET→sMF→sAML (N = 6), and ET→sAML (N = 66), respectively. Among PV patients (median F/U duration 47.4 months), 33 patients (1.36%) underwent transformation to either sMF (N = 13) or sAML (N = 20), respectively. Among pMF patients (median F/U duration 31.9 months), 81 patients (13.59%) underwent transformation to sAML. Patients whose diagnosis was changed from ET to PV during F/U showed higher transformation rate to sMF (2.41% vs. 0.53%; p = 0.0273) and a tendency of higher sAML (1.20% vs. 0.81% to sAML; p = 0.6950) compared to primary PV patients.
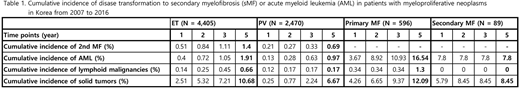
Five-year CI of transformation to sMF and sAML were 1.4% and 1.91% in ET patients, 0.69% and 0.97% in PV patients, and N/A and 16.54% in pMF patients, respectively (Table 1). Five-year CI of second lymphoid malignancies and solid cancers were 0.66% and 10.68% in ET, 0.17% and 6.67% in PV, and 1.30% and 12.09% in pMF patients, respectively (Table 1).
Although this study has relatively short F/U duration and lacks information regarding mutational status, it clearly shows that 1) transformations are common in MPNs patients in the order of pMF, ET, followed by PV. 2) Patients whose diagnosis had changed from ET to PV during F/U had a tendency of higher transformation rate: They may be true transformed PV patients who had different biologic feature to primary PV patients, or some of them might be so-called 'masked PV' patients harboring JAK2 mutation and marrow findings of PV (Barbui et al. Am J Hematol 2014). 3) Patients with ET had a significantly high risk for second solid cancers almost as those with pMF did. Longer F/U of those population and future studies by subgroup analyses of PV (primary PV vs. transformed or masked PV) and ET (ET vs. pre-fibrotic MF according to 2016 WHO criteria) would further clarify the characteristics of transformation and second cancer in MPNs patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.